Inflammatory Bowel Disease: Insights into the Enigmatic Interplay of Genetics, Immune Response, and Environmental Factors
Dr. Craig Smith, MD
4 Min read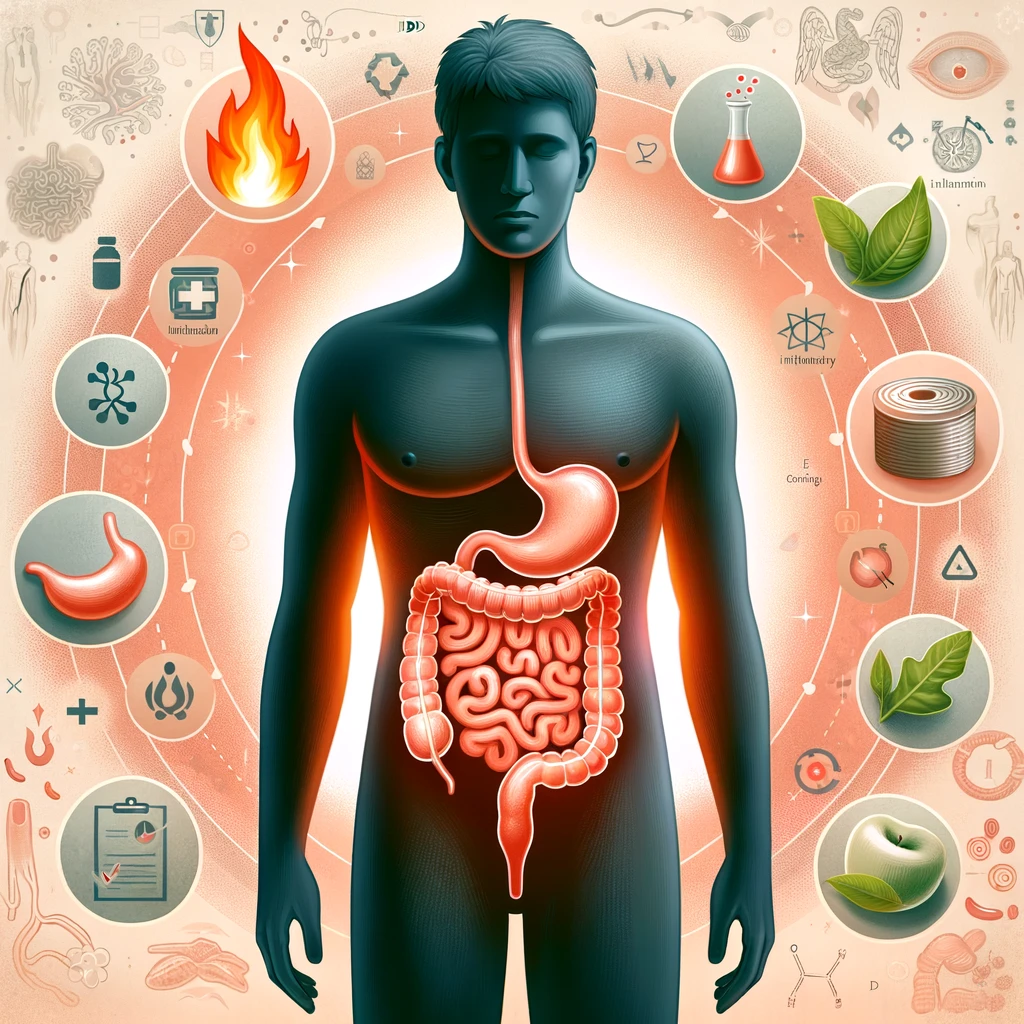
In the intricate landscape of inflammatory bowel disease (IBD), comprising conditions such as Crohn's disease and ulcerative colitis, a staggering 1.3 percent of adults in the United States grapple with chronic inflammation in the gastrointestinal (GI) tract, as reported by the Centers for Disease Control and Prevention (CDC) in 2015. This equates to approximately 3 million individuals navigating the challenges of these relentless disorders.
Unraveling the Precise Triggers of IBD:
Deciphering Autoimmune Terrain: Autoimmune diseases, a realm inhabited by over 80 identified disorders, witness the immune system mistakenly attacking healthy tissues. Recognizable names in this domain include type 1 diabetes, rheumatoid arthritis (RA), psoriasis, lupus, and multiple sclerosis. The immune system, designed as a guardian against external threats, can occasionally misfire, responding to the body's own constituents as if they were invaders.
IBD within the Immunological Tapestry: IBD finds its place under the umbrella of immune-mediated inflammatory diseases (IMIDs). IMIDs, a diverse group encompassing conditions characterized by chronic inflammation due to aberrant immune responses, include autoimmune diseases and extend to conditions like asthma and other allergies. Unlike traditional autoimmune diseases where the immune system erroneously targets healthy organs and tissues, IBD is marked by an unconventional immune response to environmental triggers in genetically predisposed individuals.
In essence, IBD emerges from an immune system gone awry, mounting a response against substances that are typically deemed harmless within the GI tract. The GI tract, replete with potential antigens such as food, medications, and beneficial bacteria known as commensals, is usually tolerated by the immune system. However, in IBD, a trigger prompts the immune system to attack these normally innocuous elements, leading to heightened and persistent inflammation in the affected GI tract.
The Role of the Immune System:
The GI tract, often overlooked in its immunological significance, houses numerous potential antigens, including commensals crucial for digestive health and immune system development. Ordinarily, the immune system tolerates these elements, recognizing them as benign and refraining from attack.
In IBD, a disruptive trigger compels the immune system to perceive these normally harmless factors as threats. Consequently, immune cells flood the GI tract, attempting to eliminate the perceived threat, inadvertently causing further inflammation and damage. Additionally, dysbiosis, an imbalance of bacteria, occurs in individuals with IBD, though whether it is a cause or effect remains unclear. This alteration in the GI tract's bacterial composition may further influence immune activity and inflammation.
Unveiling the Enigma of IBD Causes:
The exact cause of IBD remains elusive, weaving a complex tapestry involving genetic predisposition, immune responses, and environmental factors. Genetics play a pivotal role, with first-degree relatives of individuals with IBD facing up to a fivefold increased risk of developing the condition. Identified genes associated with IBD often relate to immune system regulation, maintenance of the GI tract lining, oxidative stress, and antimicrobial defenses.
Environmental factors, though not to be overlooked, have become increasingly prominent in understanding IBD. A 2019 study noted a significant global surge in IBD prevalence between 1990 and 2017, particularly in high-income countries like the United States and the United Kingdom. This underscores the potential impact of environmental risk factors in triggering or exacerbating IBD in genetically susceptible individuals. Examples of such factors include gastrointestinal infections, certain medications (like antibiotics, NSAIDs, and hormonal birth control), and dietary patterns rich in fats, sugars, or meat.
Distinguishing Crohn's Disease and Ulcerative Colitis:
IBD manifests in two distinct forms: Crohn's disease and ulcerative colitis. Crohn's disease can affect any part of the GI tract, with a predilection for the small intestine and the initial segment of the large intestine. Its progression may lead to scarring, narrowing, and fistula formation in affected areas.
On the other hand, ulcerative colitis primarily involves the large intestine, causing the formation of ulcers on its inner lining, often resulting in bloody diarrhea. Potential complications of ulcerative colitis include anemia, bowel perforation, and an increased risk of colorectal cancer.
IBD and the Spectrum of Autoimmune Diseases:
The intersection between IBD and autoimmune diseases unveils intriguing connections. Research suggests that individuals with IBD may face an elevated risk of developing autoimmune diseases. A 2016 study revealed a higher incidence of autoimmune diseases in those with IBD compared to those without, with severe IBD correlating with an increased risk of autoimmune disease. A subsequent 2017 study identified a prevalence of 20 different IMIDs in individuals with IBD, including type 1 diabetes, RA, psoriasis, celiac disease, and asthma.
Navigating IBD in the Era of COVID-19:
Addressing concerns surrounding IBD and the ongoing COVID-19 pandemic becomes paramount. Contrary to increasing one's susceptibility to the novel coronavirus, having IBD doesn't elevate the risk of contracting COVID-19 or experiencing severe illness. However, maintaining IBD in remission assumes critical importance during these times.
Continuity of IBD medications as prescribed is emphasized by healthcare authorities such as the Crohn's and Colitis Foundation. While apprehensions may arise due to the potential immunosuppressive effects of certain IBD medications, discontinuation without medical consultation is discouraged. In the event of a COVID-19 diagnosis, temporary adjustments to medication regimens may be required, underscoring the importance of medical guidance throughout.
Treatment Strategies and Management of IBD:
The overarching goal of IBD treatment revolves around reducing inflammation in the GI tract, achieving remission, and thwarting disease progression. Medications play a central role in this therapeutic approach, encompassing aminosalicylates, corticosteroids, immunosuppressants, and biologics. Beyond pharmacological interventions, other strategies such as bowel rest, surgical interventions, and dietary adjustments contribute to comprehensive IBD management.
In conclusion, IBD emerges as an immune-mediated disease, sparking persistent inflammation within the GI tract. The intricate dance of genetics, immune responses, and environmental factors orchestrates the manifestation of IBD. Though the precise causative mechanisms remain elusive, current treatments focus on mitigating GI tract inflammation to induce symptom remission. Adhering to a personalized treatment plan becomes pivotal in sustaining remission and forestalling the relentless progression of IBD.